Streptococcal pharyngitis is an infection caused by a bacteria called Streptococcus pyogenes, also called Group A Streptococcus. Recently we discussed Strep throat infections and how its complications can have devastating effects on the family.
Fortunately, this infection can be treated with antibiotics. Today I will talk about the antibiotic treatment of strep throat and what to expect if you got such a diagnosis. We arrive at strep throat diagnosis by obtaining a throat swab and sometimes going all the way to culture if the index of suspicion is high enough.
Recently we discussed Strep throat infections and how its complications can have devastating effects on the family. Fortunately, this infection can be treated with antibiotics. Today I will talk about the antibiotic treatment for strep throat and what to expect if you got such a diagnosis. We arrive at strep throat diagnosis by obtaining a throat swab and sometimes going all the way to culture if the index of suspicion is high enough.
The goals of using antibiotics to treat strep throat are to limit transmission to close contacts while reducing duration and effects of the infection and averting some of the serious complications that we discussed previously.
According to the CDC, each year between 1,100 and 1,600 people die due to invasive group A strep disease. Strep throat is not invasive and its complications are rare however we need to be aware of them as the consequences of these complications can be severe.
How is Strep Throat Infection Transmitted?:
The infection gets transmitted to people in close proximity to us especially when an infected person coughs or sneezes. Also sharing utensils with someone with an infection can transmit strep throat.

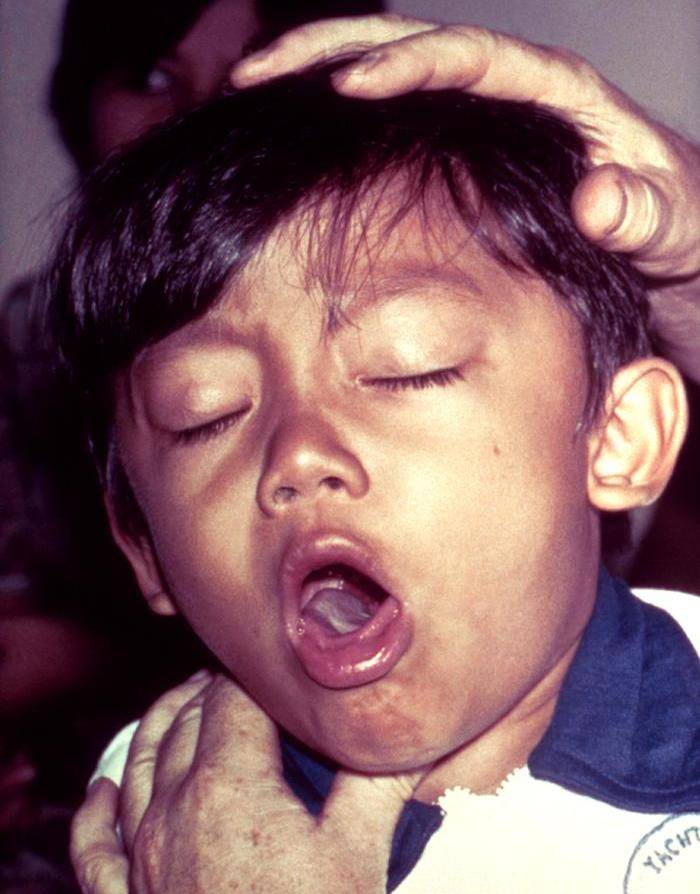
The Symptoms of Strep Throat Infection:
It is easy to mistake strep throat infection as just another viral respiratory infection. Urgent care centers often test patients for strep and make decisions based on the rapid test. The clinician, however also asks certain questions to help guide the decision making, as symptoms can and indeed do overlap between one illness and another. Below are some of the symptoms and history that the clinician identifies to make a case for or against strep throat infection.
- A sore throat that starts abruptly with painful swallowing
- Swollen lymph nodes in the neck
- Visible exudates on the posterior throat or pharynx
- Red spots on roof of mouth
- Fever
- Skin rash
- History of someone close who has been diagnosed with strep throat, usually a family member
- Headache
- Body aches
- Nausea, vomiting in the young

The Antibiotics Effect:
Antibiotics are most effective in hastening the resolution of symptoms if commenced within the first two days of symptoms. They also help reduce the infection-related complications like peritonsillar abscess and cervical lymphadenitis. One would ordinarily want to associate severity of symptoms with a higher likelihood of complications, but that has not been demonstrated in studies. In some cases, the rapid strep may be negative but the culture ends up positive after a couple of days. In fact, the patient may actually be feeling better. It is still important to treat as this will help limit transmission of the infection.
There is some research that has demonstrated recurrence of strep throat more in children who received antibiotics at the first visit compared with those who got antibiotics 48 hours later. This is believed to be because of inadequate time for the body to build up immunity for the infection. The strategy of delaying antibiotics commencement in mild to moderate recurrent infection may be helpful in reducing recurrence.
However, antibiotics cannot be purchased without a prescription; thus, the child experiencing strep throat must first see his/her doctor.
Call your physician if you or your child exhibit any of the following symptoms:
- A sore throat with tender, swollen lymph glands
- A sore throat that doesn’t go away within 48 hours
- A fever
- A sore throat with a rash
- Problems breathing or swallowing
Additionally, if your doctor has diagnosed you with strep and you don’t feel better after taking antibiotics for 48 hours, it’s crucial to follow up with your healthcare provider. These specific symptoms and scenarios highlight the importance of seeking medical attention to ensure proper treatment and recovery.
What to Do if Antibiotics Don’t Seem to Work for Strep Throat?
Sometimes, antibiotics may not seem to alleviate strep throat symptoms. In such cases, consider the following steps:
- Evaluate the Diagnosis: It’s possible that your sore throat might be caused by a virus rather than a bacterial infection. Viral infections don’t respond to antibiotics, so other treatments may be necessary.
- Consider Strep Carriers: Some people are carriers of strep bacteria but don’t exhibit symptoms. If you’ve taken the prescribed antibiotics and still have a sore throat, you might be a strep throat carrier experiencing a viral infection.
- Consult Your Doctor: If after completing the antibiotic course, your symptoms persist, it’s crucial to consult your healthcare provider. They might suggest additional tests or alternate treatments.
- Re-test: Your doctor might recommend a follow-up test to confirm whether the strep bacteria is still present. This can help in determining if a different antibiotic is required.
- Manage Symptoms: While awaiting further advice from your healthcare provider, manage symptoms with over-the-counter pain relievers, throat lozenges, and plenty of fluids.
Key Points to Remember
- Re-diagnosis: Sometimes, the initial diagnosis might need revisiting.
- Viral Infections: Antibiotics don’t work on viruses, so understanding the exact cause is crucial.
- Medical Advice: Always keep your healthcare provider in the loop for persistent symptoms.
Do Antibiotics Make Strep Throat Worse Before Making It Better?
Antibiotics are designed to combat bacterial infections, and strep throat is no exception. However, before the medication has a chance to take full effect, your symptoms might seem to worsen.
How Antibiotics Work for Strep Throat
- Timeline for Effectiveness: Antibiotics typically require 24-48 hours to begin significantly reducing the bacterial load. During this period, symptoms such as soreness, inflammation, and discomfort might temporarily intensify.
- Bacterial Elimination: As the antibiotics start to eliminate the bacteria, the immune response can cause an increased feeling of illness. This is part of the natural healing process, not a sign of effective treatment making things worse.
Short-Term Symptom Worsening
- Inflammation: The bacteria cause inflammation, which can persist or even worsen briefly before the medication takes full effect.
- Symptoms Monitoring: It’s crucial to monitor your symptoms during the first two days of antibiotic treatment.
If you do not observe improvement within 48 hours, it could indicate a different issue, such as a viral infection, which does not respond to antibiotics. In such cases, seeking medical advice is vital to determine the appropriate course of action.
Action Steps
- Start Antibiotics: Begin taking the prescribed antibiotics as directed by your healthcare provider.
- Observe: Monitor your symptoms closely over the next two days.
- Seek Further Help: If there’s no noticeable improvement after 48 hours, consult your doctor to rule out viral infections or other complications.
In summary, antibiotics do not make strep throat inherently worse—they are working toward eliminating the infection. The temporary worsening of symptoms is a typical part of the body’s response to treatment and should generally improve within a couple of days.
Antibiotic use up to 9 days after onset of symptoms has been shown to indeed reduce the occurrence of acute rheumatic fever complication of strep throat infection. The same effect has not been seen in the preventing P.A.N.D.A.S. or glomerulonephritis. The most optimal prevention is when the antibiotic coverage is for 9 to 11 days.
The transmission of strep throat infection normally is about 35% once the organisms are present in the throat. The goal of antibiotics is to eradicate throat presence of the bacteria. Good clearance is often achieved with the administration of penicillin or amoxicillin. Some studies have demonstrated between 80% and 90% clearance of throat carriage after 24 hours of penicillin or amoxicillin. However, without antibiotics, the body’s immune system eliminates throat carriage in up to 50% of infected patients after a full month.

Choice and Duration of Antibiotics Use In Strep Throat Infection:
The recommended duration of antibiotics treatment for strep throat is 10 days at least. This has been demonstrated to prevent the dreaded rheumatic fever complication. We commence treatment early since it is a form of secondary prevention. Thus by reducing transmission we are preventing others from getting strep throat. If it is not Group A strep throat, but a Group G or C then the antibiotics ought to be stopped after 5 days.
Penicillin is the antibiotic of choice. We sometimes use other related agents too like amoxicillin and ampicillin. Good but more expensive alternatives include macrolide group of antibiotics, cephalosporin group and clindamycin.
If asked, does Bactrim (trimethoprim/sulfamethoxazole) treat strep throat? Answer is, we NEVER use and do not recommend Bactrim or fluoroquinolones for the treatment of strep throat infection as they do not eradicate the organism and may further put pressure of drug resistance on the antibiotic.
Intramuscular injection of procaine penicillin was found to be effective for the antibiotic treatment of strep throat and the prevention of rheumatic fever. However, more commonly we now use Penicillin G Benzathine (Bicillin L-A). When we use the injection, it is preferred to combine it in children with procaine penicillin as Bicillin C-R 900/300. Penicillin G provides bactericidal levels against group A strep for up to 21-28 days.
Oral Penicillin V is the medicine of choice that we use to treat strep throat infection. It is given for a full 10 days. We use 250 mg two to three times a day if the child is less than 27kg in weight or 500mg two to three times a day if the child is more than 27kg.
We use 250 mg two to three times a day if the child is less than 27kg in weight or 500mg two to three times a day if the child is more than 27kg for 10 days.
Many pediatricians also use oral amoxicillin in treating strep throat and some prefer it because it has better gastrointestinal absorption and tastes better than penicillin.
Cephalosporins, usually of the first-generation can also be used, but we do not use them as first line treatment since they are much more expensive, less effctive and have a broader spectrum.
I have had some patients who have a penicillin allergy. If the allergy did not have life-threatening symptoms, I would use cephalosporins. However, if there is a higher risk of life-threatening reaction, macrolide antibiotics like azithromycin are used. The down side to macrolides is that the resistance can be as high as 20%. Bactrim should NOT BE USED for strep throat.
For the clinical symptoms, there is a scoring system that was developed and published in 1998 to help reduce the overuse of antibiotics . I have created a form here
Read a more detailed article here on the AAFP website.
What has been your experience with strep throat? Comment below or on our Facebook Page. Share this article.
Omega Pediatrics Difference: Omega Pediatrics Difference:
At Omega Pediatrics in Roswell, Georgia as well as Marietta Georgia, we understand the challenges that parents face when their children develop symptoms late in the day or after hours. Many pediatric offices are closed after 4 pm; however, we are open every weekday up to 9 pm for walk-ins, and we have telemedicine via e-visits for our known patients.
If you need treatment for strep, you may be able to use online health counseling or telehealth services to receive the diagnosis and medications you need. Many will also accept your health insurance and cover it as a part of your typical sick visits.
Why Choose Telehealth?
- Convenience: Access medical care from the comfort of your home.
- Extended Hours: Services available even after traditional office hours.
- Insurance Coverage: Many telehealth providers accept health insurance, making it a cost-effective option.
Be sure to always use a reputable online health provider. By combining the convenience of telemedicine with our extended hours, Omega Pediatrics ensures your child gets the care they need, when they need it.
Book an appointment online here
What can be done to help with the symptoms of strep throat while waiting for the antibiotics to heal the infection?
When dealing with a throat infection, antibiotics may be the definitive cure. However, there are several ways to ease the discomfort and manage symptoms naturally. Here are effective methods to help soothe a throat infection:
Home Remedies
Saltwater Gargle: Dissolve 1/4 teaspoon of table salt in eight ounces of warm water. Gargle with this mixture several times a day to reduce inflammation and kill bacteria.
Hydration and Rest: Ensure you stay well-hydrated by drinking plenty of fluids. Getting adequate rest is crucial for your immune system to combat the infection.
Soft Foods: Consume soft, easy-to-swallow foods like soups, mashed potatoes, and yogurt to minimize throat irritation.
Humidifier: Using a humidifier can keep the air moist, which helps soothe a dry and sore throat.
Over-the-Counter Solutions
Pain Relievers: Over-the-counter pain relievers like ibuprofen or acetaminophen can alleviate pain and reduce fever.
Throat Lozenges and Sprays: Medicated throat lozenges or sprays can provide immediate relief from soreness and inflammation.
Precautions for Children
When it comes to children and teenagers, be cautious with medications.
Aspirin Warning: Avoid giving aspirin to children or teens recovering from chickenpox or flu-like symptoms, as it can lead to Reye’s syndrome, a rare but serious condition. Aspirin is generally safe for children over three years old, but it’s best to consult with a healthcare professional first.
Herbal Remedies
Honey and Lemon: A mixture of honey and lemon in warm water can soothe the throat. Honey has natural antibacterial properties, while lemon provides a dose of vitamin C.
Herbal Teas: Herbal teas like chamomile or ginger tea can reduce inflammation and provide relief.
By employing these strategies, you can manage throat infection symptoms effectively and promote a quicker recovery.
Can Strep Throat Be Treated with Leftover Medications? NO!
No, it is not advisable to use leftover medications to treat strep throat. Here’s why:
Complete the Full Course of Medication
When prescribed antibiotics, it’s crucial to finish the entire course as directed by your healthcare provider. Not completing the regimen can result in the bacteria not being fully eradicated, leading to a possible recurrence of the illness.
Health Risks
Utilizing leftover antibiotics from a previous illness can pose serious health risks. The medication might not be suitable for the current infection, and improper use of antibiotics can contribute to antibiotic resistance, making future infections harder to treat.
Safety Concerns for Others
Never give leftover antibiotics to someone else, especially children. Different illnesses require different treatments, and what was effective for one condition might be harmful if used inappropriately for another.
Key Points to Remember
Always complete your prescribed antibiotic course.
Avoid using leftover antibiotics for new infections.
Consult a healthcare professional for appropriate treatment.
Do not share medications.
Using antibiotics responsibly ensures their effectiveness and safeguards your health. Always seek new prescriptions for new illnesses to ensure proper treatment and recovery.
What are the Common Misconceptions about Trimethoprim-Sulfamethoxazole for Streptococcus pyogenes (Group A Strep) Skin Infections
When it comes to treating skin and soft tissue infections, there’s a lot of misinformation surrounding the use of trimethoprim-sulfamethoxazole, particularly for infections caused by Streptococcus pyogenes (Group A Strep). Let’s clear up some of these myths:
Misconception: Ineffectiveness Against S. Pyogenes
One major misunderstanding is the belief that trimethoprim-sulfamethoxazole is ineffective against S. Pyogenes. This idea stems largely from outdated laboratory practices where the bacteria were grown on thymidine-containing agar. Such media could falsely indicate resistance because S. Pyogenes can utilize thymidine to bypass the drug’s mechanism of action.
Fact: Modern Testing Methods Confirm Effectiveness
Modern practices use thymidine-depleted media, which eliminates this issue. When tested correctly, all S. Pyogenes isolates in North America show susceptibility to trimethoprim-sulfamethoxazole, with minimum inhibitory concentrations (MICs) of ≤ 0.12 µg/ml.
Misconception: Need for Combination Therapy
Another misconception is that trimethoprim-sulfamethoxazole must be used in combination with a beta-lactam antibiotic for effective treatment. While this approach was common, recent studies have shown that trimethoprim-sulfamethoxazole alone can achieve a high cure rate for uncomplicated skin and soft tissue infections.
Fact: High Cure Rates with Monotherapy
A randomized control trial has demonstrated an 88.2% cure rate for uncomplicated skin and soft tissue infections with trimethoprim-sulfamethoxazole monotherapy. This supports its use as a first-line treatment in many cases.
Misconception: Only Effective Against Staphylococcal Infections
Finally, it’s often assumed that trimethoprim-sulfamethoxazole is only useful against staphylococcal infections and not streptococcal ones. With the rise of methicillin-resistant Staphylococcus aureus (MRSA), treatment guidelines have indeed shifted. However, this doesn’t negate the effectiveness of trimethoprim-sulfamethoxazole against S. Pyogenes when used correctly.
Fact: Versatile Use in Various Infections
Trimethoprim-sulfamethoxazole is indeed effective against both staphylococcal and streptococcal infections, making it a versatile option for various types of skin and soft tissue infections.
In summary, while there are several myths surrounding the use of trimethoprim-sulfamethoxazole for S. Pyogenes infections, modern evidence and proper laboratory techniques confirm its effectiveness. This makes it a reliable option for treating uncomplicated skin and soft tissue infections caused by both staphylococcal and streptococcal bacteria.