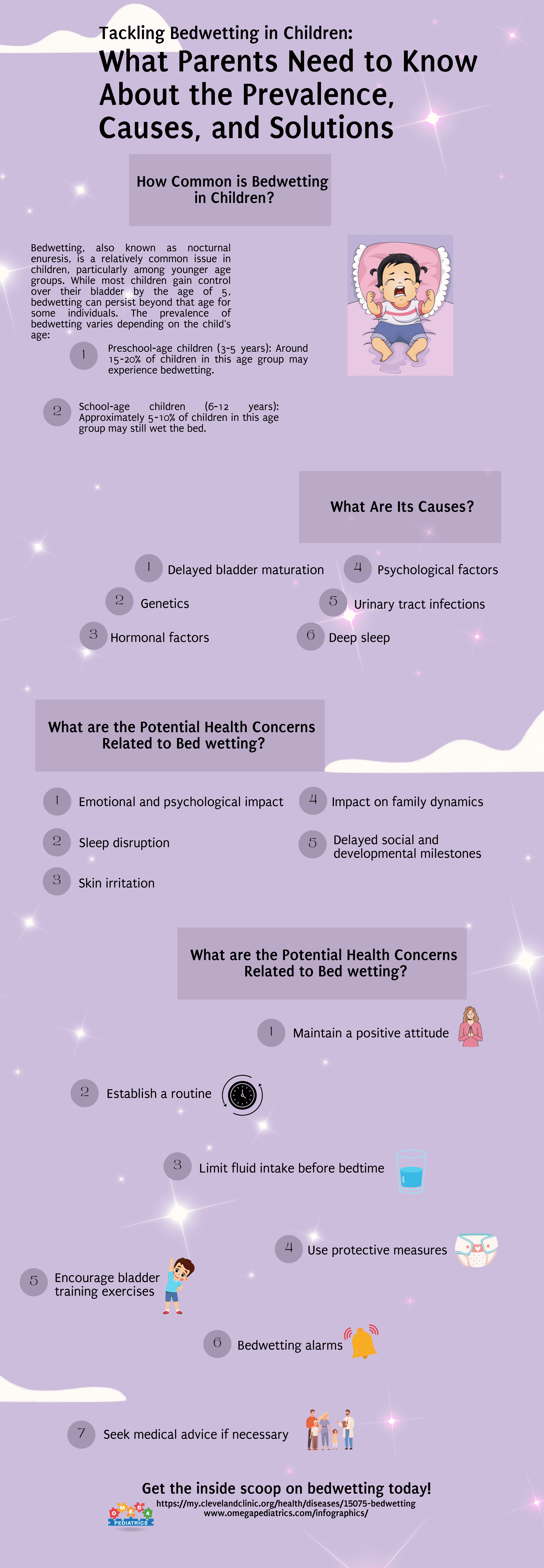
How Common is Bedwetting in Children and What Are Its Causes?
Bedwetting, also known as nocturnal enuresis, is a relatively common issue in children, particularly among younger age groups. While most children gain control over their bladder by the age of 5, bedwetting can persist beyond that age for some individuals. The prevalence of bedwetting varies depending on the child’s age:
- Preschool-age children (3-5 years): Around 15-20% of children in this age group may experience bedwetting.
- School-age children (6-12 years): Approximately 5-10% of children in this age group may still wet the bed.
What Are Its Causes?
Bedwetting can be caused by various factors, which can often interact with one another. Some of the common causes include:
- Delayed bladder maturation: Some children’s bladders take longer to develop the ability to hold urine during sleep, resulting in bedwetting.
- Genetics: Bedwetting tends to run in families. If one or both parents wet the bed as children, there is a higher likelihood that their child may experience bedwetting as well.
- Hormonal factors: The antidiuretic hormone (ADH) helps reduce urine production during sleep. Some children may produce insufficient ADH or have difficulty responding to it, leading to increased urine production and bedwetting.
- Deep sleep: Some children who wet the bed may sleep more deeply, making it difficult for them to wake up when their bladder is full.
- Urinary tract infections: Infections in the urinary system can contribute to bedwetting, although they are not a common cause.
- Psychological factors: Stressful events, emotional difficulties, or major life changes (such as moving or starting school) can occasionally trigger or exacerbate bedwetting.
What are the Potential Health Concerns Related to Bed wetting?
- Emotional and psychological impact: Bedwetting can negatively impact a child’s self-esteem, leading to feelings of embarrassment, shame, and frustration. It may affect their social interactions and cause anxiety or stress, especially when staying overnight at friends’ houses or attending sleepovers.
- Sleep disruption: Bedwetting can disturb a child’s sleep, causing them to wake up due to discomfort or wetness. This can lead to inadequate sleep, daytime sleepiness, and fatigue, affecting their overall energy levels, mood, and cognitive function.
- Skin irritation: Prolonged exposure to urine can irritate the skin, leading to rashes, redness, and discomfort. In some cases, it may result in skin infections or sores.
- Impact on family dynamics: Bedwetting can create stress and frustration within the family, particularly if parents or caregivers are struggling with managing and cleaning up after bedwetting incidents. Siblings may also be affected if they share a bedroom or have disrupted sleep due to the issue.
- Delayed social and developmental milestones: In rare cases, severe and persistent bedwetting may be associated with underlying medical conditions or developmental delays. If a child continues to wet the bed beyond the age when it is typically expected to resolve, it is important to seek medical evaluation to rule out any underlying causes.
How Can Parents Manage Bed Wetting in Children?
Managing bedwetting in children requires a supportive and understanding approach from parents. Here are some strategies that can help parents manage bedwetting effectively:
- Maintain a positive attitude: It is important for parents to approach bedwetting with empathy, reassurance, and understanding. Avoid blaming or shaming the child, as this can negatively impact their self-esteem. Let them know that bedwetting is a common issue that many children outgrow.
- Establish a routine: Encourage your child to establish a regular toileting routine before bedtime, including emptying their bladder before sleep. This can help reduce the amount of urine in their bladder during the night.
- Limit fluid intake before bedtime: Restricting the amount of fluid your child drinks in the evening, particularly caffeinated and sugary beverages, can help minimize the likelihood of bedwetting. However, ensure they still consume enough fluids throughout the day to stay hydrated.
- Use protective measures: Place a waterproof mattress cover or protective bedwetting sheets on your child’s bed to protect the mattress. This makes cleanup easier and lessens the discomfort associated with wet bedding.
- Encourage bladder training exercises: Bladder training exercises, such as scheduled voiding, can help increase the bladder’s capacity and strengthen control over urination. Gradually extend the time intervals between bathroom visits to train the bladder to hold urine for longer periods.
- Bedwetting alarms: Bedwetting alarms are devices that can sense moisture and alert the child (and/or parents) with an alarm when they begin to wet the bed. This helps train the child to wake up and respond to the sensation of a full bladder. Bedwetting alarms can be an effective intervention but require consistent use and parental involvement.
- Seek medical advice if necessary: If bedwetting persists despite trying these strategies or if it is causing significant distress to the child, it is advisable to consult a healthcare professional. They can help identify any underlying medical conditions or provide additional guidance and support.
Understanding the Role of Dietary Factors in Bedwetting
While addressing bedwetting, it’s crucial for parents to consider the potential influence of dietary factors on their child’s condition. Research suggests that certain foods and drinks may contribute to bedwetting in susceptible individuals. Although not a primary cause, dietary choices can impact bladder function and nighttime urination. Here’s a closer look at how diet may play a role:
- Caffeine and Sugary Beverages: Both caffeine and sugary drinks can act as diuretics, increasing urine production. It’s advisable to limit or eliminate the consumption of caffeinated beverages such as cola, tea, and some energy drinks. Additionally, cutting back on sugary drinks before bedtime can contribute to better bladder control.
- Fluid Intake Timing: While staying hydrated is essential for overall health, managing fluid intake in the evening can be beneficial. Encourage your child to consume most of their fluids earlier in the day, reducing the likelihood of a full bladder during the night. This approach, combined with the establishment of a consistent toileting routine, can help manage bedwetting.
- Dietary Sensitivities: Some children may have sensitivities or allergies to certain foods that can affect bladder function. Pay attention to any patterns between specific foods in their diet and episodes of bedwetting. If a connection is suspected, consulting with a healthcare professional or a registered dietitian can provide valuable insights into potential dietary modifications.
While dietary adjustments may not be a standalone solution for bedwetting, they can complement other strategies in a holistic approach to managing the condition.
Conclusion: Empowering Parents for Effective Bedwetting Management
Bedwetting can be a challenging experience for both children and parents, but it’s essential to approach it with patience, understanding, and a proactive mindset. By recognizing the prevalence and potential causes of bedwetting, parents can implement a combination of strategies to support their child effectively.
From maintaining a positive attitude and establishing routines to considering dietary factors and utilizing bedwetting alarms, parents have various tools at their disposal. Seeking medical advice when needed ensures a comprehensive approach to rule out any underlying medical conditions and receive tailored guidance.
Remember, bedwetting is a common issue that many children overcome with time and appropriate support. As parents navigate this journey, fostering open communication with their child and providing a supportive environment can make a significant difference in managing bedwetting and promoting a positive overall experience for the entire family.