In the realm of neonatal care, few conditions are as frequently encountered—and as commonly misunderstood—as jaundice. Often manifesting as a yellowing of the skin and eyes, jaundice can be a source of intense worry for new parents. I am Dr. Michael Nwaneri, a pediatrician and obesity medicine specialist, and this extensive guide aims to clarify the nuances of neonatal jaundice, outlining its causes, symptoms, diagnostic methods, and treatment options.
What is Neonatal Jaundice?
Jaundice occurs due to elevated levels of bilirubin—a yellowish substance—in the bloodstream. In newborns, the liver, which is responsible for processing bilirubin, is sometimes too immature to efficiently perform this task, leading to a buildup.
The Astonishing Epidemiology: How Common is It?
Neonatal jaundice is exceedingly common, occurring in approximately:
- 60% of full-term infants
- 80% of preterm infants
What Causes Jaundice in Newborns?
- Physiological Jaundice: The most common form, usually appears around the 2nd to 4th day of life and is generally harmless.
- Breastfeeding Jaundice: Can occur in breastfed babies due to insufficient milk intake in the first week.
- Hemolytic Jaundice: Caused by conditions like Rh or ABO incompatibility between mother and baby, leading to rapid destruction of red blood cells.
- Others: Liver malformations, infections, or enzyme deficiencies can also be underlying causes.
Identifying Jaundice: The Vital Signs
- Yellowing of the Skin: Begins on the face and progresses downwards.
- Yellowing of the Eyes: Particularly the whites of the eyes.
- Lethargy and Poor Feeding: In severe cases.
Diagnosis: An Essential Roadmap
- Visual Assessment: A basic but crucial first step.
- Blood Test: Measures bilirubin levels.
- Additional Testing: To rule out underlying conditions, such as blood type testing, complete blood count, and others.
The Path to Recovery: Treatment Options
Mild Cases:
- Increased Feeding: To help naturally eliminate bilirubin.
- Frequent Monitoring: Regular check-ups to ensure bilirubin levels are decreasing.
Moderate to Severe Cases:
- Phototherapy: Use of a special light to break down bilirubin in the skin.
- Exchange Transfusion: Rarely, severely elevated bilirubin levels may require replacement of the baby’s blood.
Preventive Measures: Guarding Your Baby’s Health
- Timely Feeding: Helps in the natural excretion of bilirubin.
- Early Diagnosis: Frequent neonatal check-ups, especially within the first 48-72 hours.
Understanding the Causes
Physiological Jaundice: The most common form of neonatal jaundice is physiological jaundice, which usually emerges around the 2nd to 4th day of life. This occurrence is generally benign and results from the natural breakdown of red blood cells in the body, releasing bilirubin that the infant’s still maturing liver struggles to process efficiently. As the liver gradually catches up with its bilirubin-processing capabilities, the jaundice typically resolves on its own without intervention.
Breastfeeding Jaundice: Another common type is breastfeeding jaundice, often linked to inadequate milk intake in the initial days of a newborn’s life. When a baby doesn’t receive enough breast milk, there is a reduction in bowel movements, leading to a decreased elimination of bilirubin. This type of jaundice can be managed by ensuring that the baby is feeding adequately, and lactation consultants can play a crucial role in supporting breastfeeding mothers.
Hemolytic Jaundice: A less common but more serious form is hemolytic jaundice, which arises from conditions such as Rh or ABO incompatibility between the mother and the baby. In such cases, the mother’s immune system attacks the baby’s red blood cells, resulting in their rapid destruction and an increased production of bilirubin. Identifying and managing these blood type incompatibilities is crucial to prevent severe jaundice and its complications.
Other Causes: In rare instances, liver malformations, infections, or enzyme deficiencies may contribute to jaundice in newborns. Comprehensive diagnostic evaluations are necessary to identify these underlying causes and initiate appropriate interventions.
Recognizing Jaundice: Vital Signs
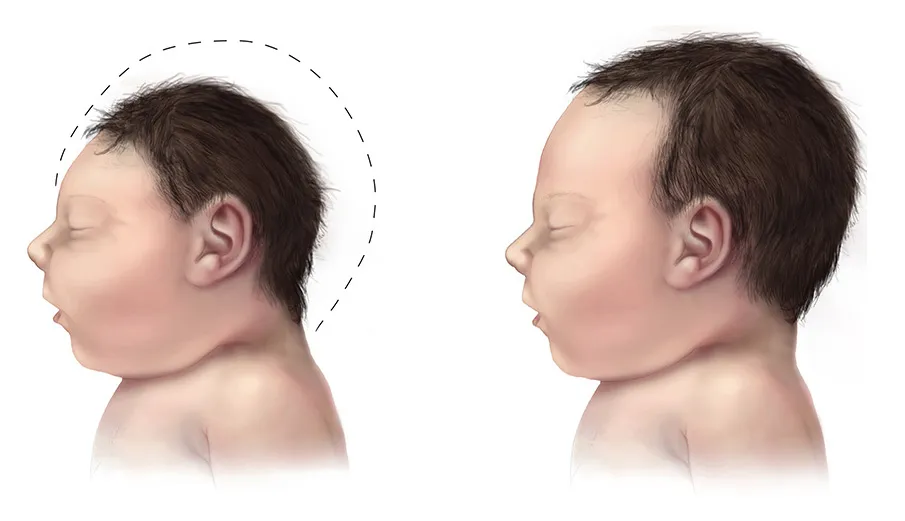
The yellowing of the skin, known as icterus, often begins on the face and progresses downwards, becoming noticeable on the chest, abdomen, and extremities. Additionally, the whites of the eyes may develop a yellowish tint, a sign known as scleral icterus. In more severe cases, infants may exhibit lethargy and poor feeding, prompting immediate attention from healthcare providers.
Diagnosing Jaundice: An Essential Roadmap
Visual Assessment: A preliminary visual assessment is a crucial first step in identifying jaundice. Healthcare professionals carefully observe the skin, eyes, and overall appearance of the newborn to gauge the severity of the condition.
Blood Test: A bilirubin blood test is the primary diagnostic tool for determining the level of bilirubin in the infant’s bloodstream. Based on the results, healthcare providers can categorize the jaundice as mild, moderate, or severe, guiding the appropriate course of action.
Additional Testing: To rule out underlying conditions contributing to jaundice, healthcare providers may conduct additional tests, including blood type testing, a complete blood count (CBC), and other specialized assessments.
The Path to Recovery: Treatment Options
Mild Cases: For mild cases of jaundice, the primary approach involves increasing feeding frequency. This helps stimulate bowel movements, aiding in the natural elimination of bilirubin from the body. Regular monitoring through check-ups ensures that bilirubin levels are decreasing as expected.
Moderate to Severe Cases: Phototherapy is a common treatment for moderate to severe jaundice. Special lights, often blue or white, are used to expose the baby’s skin to light, which helps break down bilirubin into a form that can be easily excreted. In extreme cases with dangerously high bilirubin levels, an exchange transfusion may be considered. This procedure involves replacing a portion of the baby’s blood with donor blood to rapidly reduce bilirubin concentrations.
Preventive Measures: Guarding Your Baby’s Health
Timely Feeding: Ensuring that newborns receive timely and adequate feeding is crucial for the natural excretion of bilirubin. Frequent breastfeeding or formula feeding supports healthy digestion and helps prevent jaundice, especially in the early days of life.
Early Diagnosis: Regular neonatal check-ups, particularly within the first 48-72 hours after birth, play a pivotal role in early jaundice detection. Close monitoring by healthcare professionals allows for timely intervention and reduces the risk of complications associated with severe jaundice.
In the next section, we will delve deeper into the nuances of treatment options and long-term considerations for neonatal jaundice. Understanding the importance of early intervention and ongoing care is paramount in ensuring the well-being of newborns affected by this common yet often misunderstood condition.
Treatment Modalities and Long-Term Considerations
Phototherapy: In cases where jaundice requires intervention, phototherapy is a widely employed treatment. This involves exposing the baby’s skin to specific wavelengths of light, which facilitate the breakdown of bilirubin into forms that can be excreted more easily. Phototherapy is typically administered in a hospital setting, and infants may be placed under special lights while wearing protective eye covers.
Exchange Transfusion: Although rare, severe cases of jaundice may necessitate more aggressive measures, such as an exchange transfusion. This procedure involves gradually replacing a portion of the baby’s blood with donor blood to rapidly reduce bilirubin levels. Exchange transfusions are meticulously performed under controlled conditions due to their complexity and potential risks.
Monitoring and Follow-up: Regardless of the treatment modality, continuous monitoring is essential. Healthcare providers closely track bilirubin levels to ensure they are decreasing at an appropriate rate. Regular check-ups also allow for the assessment of overall infant health and the identification of any potential complications.
Parental Education and Support: Educating parents about neonatal jaundice is a crucial aspect of the care process. Providing information on the causes, symptoms, and treatment options empowers parents to actively participate in their child’s care. Moreover, addressing concerns and providing emotional support can alleviate the anxiety often associated with jaundice in newborns.
Long-Term Implications: In most cases, neonatal jaundice resolves without causing long-term harm. However, certain risk factors, such as extreme prematurity or severe hemolytic jaundice, may be associated with a higher likelihood of complications. Long-term follow-up care is particularly important for infants with underlying conditions, ensuring that any potential issues are promptly addressed.

Preventive Measures and Lifestyle Factors
While neonatal jaundice is often unavoidable, there are measures parents can take to reduce the risk and severity of the condition:
- Optimal Feeding Practices: Ensuring that newborns receive sufficient breast milk or formula is crucial. Early and frequent feeding supports healthy digestion and helps prevent the buildup of bilirubin.
- Regular Neonatal Check-ups: Early detection is key. Regular check-ups within the first few days of life enable healthcare providers to monitor bilirubin levels and identify jaundice promptly.
- Addressing Underlying Conditions: If the jaundice is associated with conditions such as blood type incompatibility or enzyme deficiencies, addressing these issues early on can prevent complications.
- Skin-to-Skin Contact: Encouraging skin-to-skin contact between the baby and parents can promote bonding and facilitate breastfeeding, contributing to overall well-being.
In the next section, we will explore the emotional and psychological aspects of neonatal jaundice, acknowledging the impact it can have on parents and caregivers. Understanding the holistic needs of families facing neonatal jaundice is essential for comprehensive and compassionate healthcare delivery.
Emotional and Psychological Considerations
The experience of neonatal jaundice can be emotionally challenging for parents and caregivers. The initial concerns about the baby’s health, coupled with the need for medical interventions, can lead to stress and anxiety. Acknowledging and addressing the emotional aspects of this journey is integral to providing holistic care.
- Parental Education and Counseling: Offering comprehensive education and counseling services can empower parents to navigate the challenges associated with neonatal jaundice. Understanding the condition, its causes, and the available treatment options can alleviate anxiety and promote a sense of control.
- Support Groups and Resources: Connecting parents with support groups and resources can be invaluable. Sharing experiences with others who have gone through similar situations creates a sense of community and normalizes the emotional responses to a neonatal jaundice diagnosis.
- Open Communication with Healthcare Providers: Establishing open lines of communication between parents and healthcare providers is crucial. Regular updates on the baby’s progress, explanations of treatment plans, and addressing any concerns promptly can help build trust and alleviate anxiety.
- Postpartum Mental Health: Neonatal jaundice is often experienced during the already challenging postpartum period. Monitoring and addressing postpartum mental health, including potential feelings of guilt or inadequacy, is essential. Healthcare providers should be attuned to the emotional well-being of parents and offer appropriate support.
Conclusion: Navigating the Maze of Neonatal Jaundice
While the initial discovery of jaundice in your newborn can be distressing, understanding the condition can go a long way in mitigating fears and ensuring the best possible outcome for your baby.
References:
- American Academy of Pediatrics – Guidelines on Neonatal Jaundice
- National Institutes of Health – Neonatal Jaundice
- Mayo Clinic – Newborn Jaundice
Disclaimer: This guide is for educational purposes and should not replace professional medical advice.