Childhood obesity is increasingly prevalent nowadays. Obese children under five years old have increased from 32 million in 1990 to 41 million in 2016, according to the World Health Organization (WHO). These numbers are alarming!
The prevalence rate affects more than 18% of the pediatric age group, making it the most common chronic disease in childhood.
It’s important to search for ways to combat childhood obesity. Nonetheless, telemedicine interventions have become a prevalent solution. In this article, we’ll explore how effective telemedicine interventions can be to address childhood obesity.
How does Telemedicine Work?
Telemedicine in healthcare offers remote telecommunication and information technologies. It helps in the consultation, diagnosis, and drawing up of treatment plans. Video conferencing, mobile apps, and remote monitoring devices are the avenues for delivering telemedicine interventions.
What is Childhood Obesity?
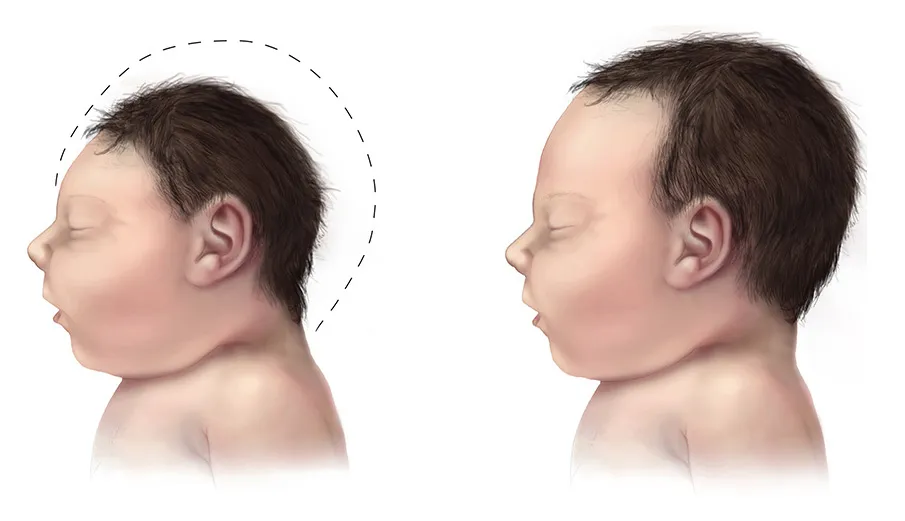
Your kid is said to be obese when his weight gain doesn’t conform to his height and weight. The Centers for Disease Control and Prevention’s (CDC) specific growth charts are the basis of weight gain data.

Childhood obesity also measures the body mass index (BMI). The figure should be above the 95th percentile mark.
Childhood obesity affects the pediatric population. Excess weight gain is medically unpleasant and should be seriously looked into. The risk factors point to behavior, genetics, and taking specific medications. The school and community can also be contributing factors.
The environment, such as the childcare facility and neighborhood layout, can contribute to children’s obesity. And lastly, access to affordable foods and beverages significantly impacts obesity among children.
Overweight children face various health risks, including the likelihood of developing diabetes, high blood pressure, high cholesterol, asthma, and sleep apnea. To prevent these serious medical conditions, parents must foster healthy eating and active lifestyles.
Healthcare systems and your provider at Omega Pediatrics can provide support and guidance to parents to prevent childhood obesity. They can provide professional counseling and advice on how to implement strategies to promote a healthy and active lifestyle for children.
Telemedicine and Childhood Obesity
Telemedicine interventions have proven successful in managing various chronic diseases, like obesity. Managing childhood obesity is a complex condition. It requires a multidisciplinary approach for effective management.
Telemedicine interventions facilitate the coordination of care, family support, and education. It can be customized to each child’s and family’s particular needs.
A telemedicine intervention for an obese child consists of a physical therapist, a psychologist, and regular video consultations with a dietitian. The child’s progress can be monitored through remote monitoring devices such as weight scales and activity trackers.
Families can be educated and supported through telemedicine interventions. This includes receiving regular educational materials such as exercise plans and healthy recipes. In addition, families who are experiencing similar challenges can join support groups.
Telemedicine and Childhood Obesity: The Benefits
The management of childhood obesity can benefit from telemedicine interventions in many ways.
Improved Access to Care
Children with obesity who live in remote areas do not have easy access to medical professionals. These kids can access medical professionals through telemedicine interventions from the comfort of their homes.
Well-Coordinated Care
Using telemedicine to coordinate care among medical experts can be improved. A multidisciplinary approach is necessary to treat childhood obesity. Telemedicine can help healthcare professionals from various specialties communicate and work together.
Enhance Patient Outcomes
Telemedicine interventions help obese children lose weight more successfully. According to a study in the Journal of Telemedicine and Telecare, telemedicine treatment for obese children significantly reduced BMI compared to a control group.
Information and Support for Families
Families need education and support to make the necessary changes to their lifestyles because childhood obesity is a complex condition that requires lifestyle changes. Interventions in telemedicine give families the tools to make these adjustments.
Cost-Effective
Telehealth treatments are economical and offer cost-effective care for childhood obesity. Interventions through telemedicine can reduce the need for in-person visits, which saves families time and money.
Telemedicine and Childhood Obesity: The Challenges
While telemedicine interventions have several benefits in the management of childhood obesity, they also face several challenges.
Access to Technology
There’s a need for technological infrastructure that includes internet connectivity and software, along with proficient medical staff capable of delivering the intervention effectively. These requirements may be a challenge in some areas.
Superficial Relationship
Telemedicine interventions lack the personal touch of in-person visits. Some families may prefer the interpersonal interactions that occur during in-person visits, which aren’t possible during telemedicine consultations.
Insurance Coverage
There’s a need for reimbursement. Telemedicine isn’t included in insurance coverage, which limits some families’ access. However, insurance providers are starting to acknowledge the advantages of telemedicine; hence, they can cover the service.
Universal Applicability
Interventions through telemedicine might not be suitable for all families. It may not be a good option for many families since they prefer in-person visits. Also, many families have limited digital literacy, which impacts their participation in telemedicine interventions.
Moreover, the intervention could be adversely affected by cultural or linguistic barriers, which pose a challenge for diverse populations.
Data Security
Nonetheless, privacy and security concerns are also challenges with telemedicine interventions. Healthcare providers need to ensure that patient data is protected when utilizing telemedicine technologies.
Telemedicine and Childhood Obesity: Ethical Considerations
Telemedicine can enhance patient outcomes, but with this new form of treatment come various ethical factors that must not be overlooked.
Access to Technology
Certain patients, such as those in remote or rural areas or those with mobility or transportation difficulties, may find telemedicine interventions more accessible. However, others who aren’t comfortable with remote care or lack technology access may be hindered.
Healthcare providers must guarantee that all patients can access telemedicine interventions, regardless of their location or background.
Likelihood of Misdiagnosis
Virtual medical interventions may not be effective enough to administer a complete physical examination or accurately pinpoint certain conditions. Physicians who utilize telemedicine must be mindful of its limitations to ensure they provide appropriate care.
Confidentiality of Data
Preserving patient confidentiality is the most vital ethical issue. Safeguards must be implemented to ensure that personal information stays secure and away from unauthorized access.
Also, healthcare professionals must adhere to rules and regulations for digital privacy protection.
Patient Education
Medical providers shall educate their patients on the potential associated risks and provide them with the option to decline remote treatment if they’re not comfortable with the service.
In addition, patients should be informed of the limitations of telemedicine. They must have clear instructions on how to seek emergency assistance.
Integrity of Care
Healthcare providers should maintain the integrity of care when utilizing telemedicine. Providers must be equipped with effective training on telemedicine technology and knowledgeable about the benefits and drawbacks of remote care.
Telemedicine—A Cost-Effective Solution Against Childhood Obesity
Studies have investigated telemedicine’s ability to tackle childhood obesity while being financially responsible. Telemedicine interventions have proven to promote healthy lifestyle habits in children, which include increasing physical activity and choosing healthy food.
A specific study indicated that employing telemedicine for weight management programs is less expensive than traditional in-person alternatives. Telemedicine interventions were linked to lower body mass index (BMI) readings when compared to standard care.
After analyzing telemedicine interventions aimed at addressing childhood obesity, researchers concluded that these interventions successfully lowered BMI levels and encouraged healthy lifestyle habits.
Telemedicine and Childhood Obesity: Parents Get Involved
Effective telemedicine interventions rely on several aspects, one of which is the active participation of parents. The engagement of parents plays a fundamental role in molding the health behaviors and lifestyle preferences of their children.
The treatment of childhood obesity through telemedicine involves virtual meetings with healthcare professionals, advising on dietary and physical exercise regimens, and monitoring the child’s progress.
Parental involvement may include the following:
- remotely attending consultations with the child
- check on their child’s diet and physical activity routine
- motivate their children to fulfill their health objectives
Parental involvement in telemedicine interventions improves the results. For instance, a study published in the Journal of Medical Internet Research found that parental involvement resulted in positive outcomes.
Parents who were actively involved in the program had higher levels of satisfaction with the intervention.
However, parental involvement also poses some challenges. These challenges are:
- Several parents lack the knowledge to support their children’s health goals
- Several parents face barriers, such as time constraints and work responsibilities. These barriers hinder their ability to participate in telemedicine interventions.
Nonetheless, telemedicine interventions should be designed to facilitate parental involvement. It should provide parents with the necessary resources, including educational materials. or involve them in the development of personalized health programs.

Boost an Active Lifestyle to Prevent Childhood Obesity
Childhood obesity is a complex condition that needs various approaches for effective management. Telemedicine interventions can facilitate the coordination of care by healthcare professionals. It provides education and support for families.
Telemedicine has proven to be a cost-effective alternative to managing obesity in children. There are time and money savings since in-person visits are greatly reduced while accurate monitoring is achieved remotely.
We at Omega Pediatrics would be glad to assist parents with the proper support, counseling, and advice to prevent obesity among our young patients. We’re sure you don’t want your kids to experience complex health conditions later.
Let’s work together for a healthy and active lifestyle for our children to combat childhood obesity.